肿瘤:“问倒老师系列”之七:股骨近端病理骨折

单纯骨囊肿
自从1876年Virchow首次报道后,单纯骨囊肿逐渐被人们认知。单纯骨囊肿为累及管状骨及扁平骨,并致局部膨胀、菲薄的骨皮质内充满浆液的瘤样病变。80%病例发现于3-14岁儿童,平均年龄为9岁。约占骨骼肿瘤的3%,男:女约为2-3:1。
病理生理:
单纯骨囊肿的病因尚不明确,目前较为认可的病因理论是Cohen提出的骨内静脉回流障碍学说,骨内静脉回流障碍导致骨内高压,增加破骨活性,致局部骨质破坏。
自然史:
单纯骨囊肿最初发生于临近骺板的干骺端,随生长发育逐渐远离骺板。临近骺板的病变常表现出更强的活动性,和远离骺板的病变相比,更容易进展和复发。临近骺板的活动性骨囊肿可能会影响长管状骨的纵向生长。10岁前发病者,囊肿多距骺板较近,可能为活动性的,10岁后发病者,病变多远离骺板,多逐渐转为静止,骺板闭合后骨囊肿很少再进展。
临床表现:
骨囊肿起初常无症状,临近关节可出现疼痛、肿胀及活动受限,发生于表浅骨骼者可触及局部骨骼膨隆、局部压痛,部分病例在发生病理骨折时,或在拍摄X线片时偶然发现。病理性骨折为本病最常见并发症,发生率约66%。部分病例因病变局部受力异常发生肢体畸形。
解剖因素:
单纯骨囊肿可累及管状骨及扁平骨,约94%单纯骨囊肿发生于肱骨及股骨近端,且肱骨发病率比股骨高2-3倍。其他可累及骨还有跟骨(2%)、髂骨(2%)、距骨及胫骨等。发生于扁平骨的病例,年龄多>12-17岁,因其病变部位较深且多无症状,故发现较晚。
诊断方法:
X线片:病变可累及长骨干骺端或骨干,极少累及骨骺,典型病例常表现为局部骨髓腔中心性膨胀,X线透射率增高,周围由薄层骨质包裹,边界清楚,囊肿纵轴常大于其横径,且囊肿横径常小于相邻骺板宽度;除非发生病理性骨折,周围常无骨膜反应。囊肿不会突破骨皮质、层状骨膜反应及Codman三角。
“落叶征”:是多房型骨囊肿的特殊X线表现。当发生病理性骨折时,一侧菲薄的骨皮质断裂形成游离骨块,并坠入囊腔内(常未充满液体),骨块浮于液面,也可部分浸入液体内。多见于骨骼成熟或邻近成熟病例。
CT:通常X线片即可提供诊断骨囊肿的充足信息,但CT扫描有助于评估所有部位的骨囊肿,尤其是骨盆骨囊肿。当囊肿发生于骨干中间或非典型部位时,CT可充分显示病变累及范围。
MRI:典型骨囊肿常表现为均一短T1及长T2信号。但这很难鉴别小于8岁患儿的单纯骨囊肿及动脉瘤样骨囊肿。
穿刺取活检:对于年龄<10岁患儿,无论单纯骨囊肿还是动脉瘤样骨囊肿均可穿出血性液体,故穿刺并非诊断单纯骨囊肿的可靠手段。有极少小年龄病例,特别是<5岁者,单纯骨囊肿可突破骺板。
囊肿肉眼观:
囊肿内可为单房,或多个不完整间隔分开的多房囊肿,其间隔被证实为正常骨质。囊腔内充满淡黄色、低粘性的浆液。经分析该浆液内含有前列腺素(特别是前列腺素E),白介素1β及蛋白酶,如胶原蛋白酶等。这些成分可介导增加破骨活性。
鉴别诊断:
动脉瘤样骨囊肿:X线片示病变扩张程度及骨皮质菲薄程度及发病部位可能有利于鉴别,动脉瘤样骨囊肿多为偏心性,常扩张更明显,且囊内可见斑片状或点状钙化。动脉瘤样骨囊肿呈多房性且MRI可显示液-液平面。穿刺囊内为不凝血。患者常有进行性局部疼痛、肿胀。
骨巨细胞瘤:多见于成人。局部痛性肿块为主要症状。病变常见于长骨骨骺。X线片显示为偏心性、膨胀性溶骨性破坏。
骨纤维异样增殖症:股骨颈及肱骨近端纤维异样增殖症继发骨囊肿者并不少见。囊肿周围骨异常膨胀、呈毛玻璃样、囊肿周围硬化骨壳较单纯骨囊肿宽改变利于鉴别。小儿病例常见于多骨型FD。
骨肉瘤:单纯溶骨肉瘤可误诊为骨囊肿。一些骨肉瘤变异或形成假包囊时,较少出现临床症状,影像学表现类似骨囊肿。在影像学上毛细血管扩张型骨肉瘤、Ewing肉瘤也可类似于骨囊肿,但这些恶性肿瘤常表现出更强的侵袭性。
治疗:
治疗的目的在于预防所有可能的并发症及肢体功能障碍。目前单纯骨囊肿尚无统一的首选治疗方法。
单纯植骨:因其较高的复发率(12%-45%),已很少采用。
刮除植骨:行囊内刮除后植骨大大提高了囊肿愈合率,但手术创伤较大,并发症较多,如术中及术后骨折等。
经皮穿刺局部注射激素:最早由Scaglietti报道,其病例成功率可达90%。该方法因其效果可观、操作相对简单、并发症较少,应用较为广泛,但多数病例需反复多次注射直至病灶完全吸收或趋于稳定。该方法是70-90年代治疗肱骨骨囊肿的最流行方法。
经皮穿刺自体骨髓移植:近些年,有研究用自体骨髓替代激素作为穿刺注射物,证实自身骨髓对诱导成骨有一定的优势,在一定程度上缩短病程,减少了注射次数。
治疗理念:
通过多因素研究分析证实,影响治疗成功与否的关键因素是患者年龄,无论选择何种治疗方法,>10岁患者成功率(90%)远高于<10岁患者(60%)。
无论治疗与否,在骨骼成熟后,囊肿趋于稳定,但病变部位无法转为影像学正常骨骼。治疗骨囊肿的目标是中止进行性的骨质破坏,获得可正常受力的、功能上稳定的骨骼,而非追求正常的X线表现。有学者认为90%的单纯骨囊肿可保守治疗。
相反,若囊肿累及承重关键部位(如股骨颈、跟骨),且有较高风险发生病理骨折时,或经系列X线片随访证实即将发生病理骨折时应积极手术治疗。
需强调的是,在尝试任何手术或穿刺注射治疗前应确保病理骨折以愈合;但对移位的股骨颈或跟骨后柱病理骨折,可行切开复位内固定以恢复正常血运及解剖完整性以降低远期功能障碍。
Senior doctor: Manuel Cassiano Neves MD, MSc (EFORT President 2013-2014)
EFORT: European Federation of National Associations of Orthopaedics and Traumatology
…………………………………………………………


10 y/o boy (otherwise healthy) complaints of R hip pain after falling on the ground, no relevant history previously.
PE: R hip limited range of motion with local tenderness.
Junior doctor: Which imaging do we need for further differential diagnosis at this moment (3 days after injury)? Is MRI helpful for differential diagnosis with aneurysmal bone cyst at this time?
Senior doctor: It looks to me this is a unicameral bone cyst (from the X-ray and CT scan) but as always I like to have a confirmation. For ABC you will see different cavities with liquid inside... but in case it will be difficult to have an MRI I would stay with the CT scan already done.
I do not think you need any further image BUT YOU NEED TO DO A BIOPSY AT THE TIME OF SURGERY.
Junior doctor:For this kind of cyst lesion, how to do the biopsy? You mean "needle aspiration" with a needle? Can we get a definite diagnosis with biopsy?
Senior doctor: Yes usually I aspirate with a needle and if it an exsudate for sure it will be a cyst if it comes blood you have to think about an aneurysmal bone cyst. The treatment for ABC I recommend primarily curettage and bone grafting but with high percentage of recurrence. This is why I treat both lesions in the same way at first attempt.
Junior doctor: What’s your treatment plan?
Senior doctor: The fracture is in varus and one of the complication will be mal-union or non-union or recurrence of the cyst.
So I suggest: Put the child on a fracture table under GA and put the femoral neck in valgus. Do a curettage by a percutaneous incision. Stabilize the fracture with internal fixation. In this particular case where we have a big cyst almost going to the growth plate it is not easy for stabilization. Since is already 10 years of age I would not mind to cross the growth plate... (in the worst scenario you can always make an epiphysiodesis in the contra-lateral side). By crossing the growth plate you will gain better stabilization!
Junior doctor: Can we consider internal fixation for this child, if so, which kind of instrument you would like to select?
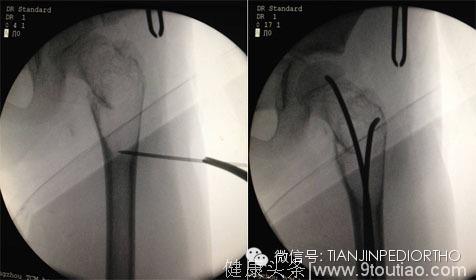
Senior doctor: Definitely in this particular case I will use ELASTIC NAILS and will complement it with an injection of Metilprednisolone according to Campannacci.
Junior doctor: Do you think skeletal traction will be just ok?
Senior doctor: As I said this fracture is prone to complications so I will definitively would not treat just with traction.
Junior doctor: If it is aneurysmal bone cyst, do you still consider ESIN to stabilize/cure it? What's your treatment strategy for aneurysmal bone cyst with fracture?
Senior doctor:If it recurrs I will do an open procedure to excise the membrane, use alchool to "burn" the surface, bone grafting and stabilization probably in this case with a special AO plate for the proximal femur (LCP) with locking screws. But I am confident that the ESIN initial approach will be enough (in my experience in this region - 9 cases all healed with this method.
Junior doctor: How do you think of the results?
Senior doctor: The x-rays look fine to me so let's wait. Just one simple technical note. Since the fracture is very high sometimes I put the 2 anisl in the femroal neck instead of one in the trochanteric region... but it's up to the surgeon to decide.
…………………………………………………………………………………………
Ulici A, Balanescu R, Topor L, et al. The modern treatment of the simple bone cysts.J Med Life. 2012 Dec 15;5(4):469-73. Epub 2012 Dec 25.
Norman A, Schiffman M.Simple bone cyst :factors of age dependecy. Radiology. 1997;124:779-782.
Conway WF, Hayes CW.Miscellaneous lesion of bone. Radiol. Clin. North Am. 1993;31:339-358.
Rafath Baig,and John L. Eady. Unicameral (Simple) Bone Cysts.South Med J. 2006 Sep;99(9):966-76.
Hunt KJ, Bergeson A, Coffin CM, et al. Percutaneous curettage and bone grafting for humeral simple bone cysts.Orthopedics. 2009 Feb;32(2):89.
A. L. Baert, Leuven,M. Knauth, G?ttingen et al. Imaging of Bone Tumors and Tumor Like Lesions -Techniques and Applications. 2009