各大指南都点名的血糖波动,该如何用于临床?
 随着持续葡萄糖监测(CGM)技术的革新与成熟,糖尿病患者的血糖监测逐渐“点动成线”——不仅能够描述患者瞬时的血糖数值,更能够描述患者一段时间内(数小时、全天甚至数月)的血糖波动、变化情况。描述血糖波动的指标——血糖稳定在目标范围内的时间(TIR)被美国糖尿病协会(ADA)、中华医学会糖尿病学分会(CDS)先后纳入指南,似乎也在提示临床医生,重视患者的血糖波动!所以,血糖波动会成为未来糖尿病管理的新靶点吗?如果要管理患者的血糖波动,临床医生该做什么?在刚刚结束的中华医学会糖尿病学分会第二十四次全国学术会议(CDS 2020)上,来自南京市第一医院内分泌科主任马建华教授从血糖波动与β细胞的关系入手,回答了上面两个问题。
随着持续葡萄糖监测(CGM)技术的革新与成熟,糖尿病患者的血糖监测逐渐“点动成线”——不仅能够描述患者瞬时的血糖数值,更能够描述患者一段时间内(数小时、全天甚至数月)的血糖波动、变化情况。描述血糖波动的指标——血糖稳定在目标范围内的时间(TIR)被美国糖尿病协会(ADA)、中华医学会糖尿病学分会(CDS)先后纳入指南,似乎也在提示临床医生,重视患者的血糖波动!所以,血糖波动会成为未来糖尿病管理的新靶点吗?如果要管理患者的血糖波动,临床医生该做什么?在刚刚结束的中华医学会糖尿病学分会第二十四次全国学术会议(CDS 2020)上,来自南京市第一医院内分泌科主任马建华教授从血糖波动与β细胞的关系入手,回答了上面两个问题。 马建华教授演讲//1//为什么要重视血糖波动?人体血糖波动的相关因素众多,而在糖尿病管理中,最相关的一项指标就是β细胞功能。国内外相关研究均证实了血糖波动对β细胞功能的预测性——血糖波动越大,β细胞功能越差。
马建华教授演讲//1//为什么要重视血糖波动?人体血糖波动的相关因素众多,而在糖尿病管理中,最相关的一项指标就是β细胞功能。国内外相关研究均证实了血糖波动对β细胞功能的预测性——血糖波动越大,β细胞功能越差。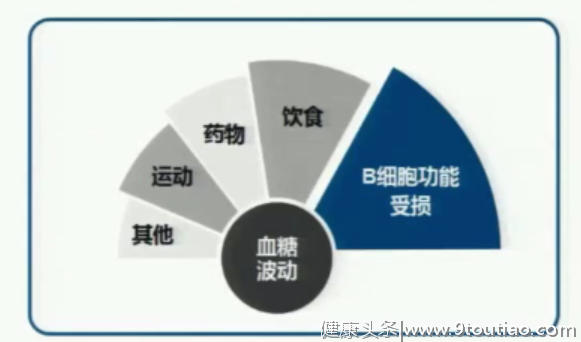 影响血糖波动的相关因素研究表明,血糖波动增加与β细胞功能降低之间存在恶性循环关系。一方面,β细胞功能减退甚至衰竭,导致胰岛素缺乏,增加了血糖的波动性;另一方面,血糖波动甚至比持续的高血糖状态更能够加剧患者的氧化应激反应,从而促进β细胞凋亡……
影响血糖波动的相关因素研究表明,血糖波动增加与β细胞功能降低之间存在恶性循环关系。一方面,β细胞功能减退甚至衰竭,导致胰岛素缺乏,增加了血糖的波动性;另一方面,血糖波动甚至比持续的高血糖状态更能够加剧患者的氧化应激反应,从而促进β细胞凋亡…… 血糖波动与β细胞功能之间的关系长久以来,患者的β细胞功能保护一直是临床管理的“盲区”,很大一部分原因是临床医生缺乏合适的可量化靶点,而当我们理清其与血糖波动的关系,管理靶点似乎呼之欲出了。马建华教授表示:“改善患者血糖波动,能够保护其残存的β细胞功能。”//2//
血糖波动与β细胞功能之间的关系长久以来,患者的β细胞功能保护一直是临床管理的“盲区”,很大一部分原因是临床医生缺乏合适的可量化靶点,而当我们理清其与血糖波动的关系,管理靶点似乎呼之欲出了。马建华教授表示:“改善患者血糖波动,能够保护其残存的β细胞功能。”//2//管理血糖波动的4大策略随着TIR被权威指南纳入,血糖波动的管理也逐渐有据可依。马建华教授系统介绍了目前血糖波动管理的4大策略,并罗列了相关研究证据:
1.胰岛素强化治疗:
新诊断2型糖尿病患者早期应用胰岛素强化治疗,可显著改善血糖波动、改善β细胞功能[1-2]。
较长病程患者应用短期胰岛素强化治疗同样能够改善β细胞功能[3]。
持续胰岛素皮下注射(CSII)和多次皮下胰岛素注射(MSII)相比,改善β细胞功能更显著[4]。
闭环胰岛素泵系统相比传统胰岛素泵,更能改善血糖波动[5]。
胰高血糖素样肽-1受体激动剂(GLP-1 RA)[6]、钠葡萄糖共转运蛋白-2抑制剂(SGLT-2i)[7]、二肽激肽酶-4抑制剂(DPP-4i)[8]也有能够改善2型糖尿病患者的血糖波动的相关证据。
一部分新型降糖药物即使在胰岛素控制血糖不佳的患者身上,仍能带来血糖波动方面的获益[9-10]。
4.胰岛移植和干细胞治疗:胰岛移植和间充质干细胞移植对血糖波动的改善已经在人体和动物研究中获得了验证[12-13]对于临床医生来说,前两大策略明显证据更多、可能性也更高,在演讲的最后,马建华教授呼吁,血糖波动和患者的β细胞功能息息相关,临床管理中一定要引起重视。
参考文献:
[1]Zhou J, Jia W, Bao Y, Ma X, Lu W, Li H, Hu C, Xiang K. Glycemic variability and its responses to intensive insulin treatment in newly diagnosed type 2 diabetes. Med Sci Monit. 2008 Nov;14(11):CR552-8. PMID: 18971871.[2]Weng J, Li Y, Xu W, Shi L, Zhang Q, Zhu D, Hu Y, Zhou Z, Yan X, Tian H, Ran X, Luo Z, Xian J, Yan L, Li F, Zeng L, Chen Y, Yang L, Yan S, Liu J, Li M, Fu Z, Cheng H. Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet. 2008 May 24;371(9626):1753-60. doi: 10.1016/S0140-6736(08)60762-X. PMID: 18502299.[3]Liu L, Yang S, Liu J, Li H, Liu J, Cao X, Xiao H, Li Y. Fasting Plasma Glucose Indicates Reversibility of the Acute Insulin Response after Short-Term Intensive Insulin Therapy in Patients with Various Duration of Type 2 Diabetes. J Diabetes Res. 2018 Nov 15;2018:9423965. doi: 10.1155/2018/9423965. PMID: 30581872; PMCID: PMC6276474.[4]区洪炎, 罗导航, 刘娟,等. 不同胰岛素强化治疗时间和模式对2型糖尿病患者胰岛β细胞功能影响的研究[J]. 中国糖尿病杂志, 2019, 27(05):326-330.
[5]Hovorka R, Kumareswaran K, Harris J, Allen JM, Elleri D, Xing D, Kollman C, Nodale M, Murphy HR, Dunger DB, Amiel SA, Heller SR, Wilinska ME, Evans ML. Overnight closed loop insulin delivery (artificial pancreas) in adults with type 1 diabetes: crossover randomised controlled studies. BMJ. 2011 Apr 13;342:d1855. doi: 10.1136/bmj.d1855. PMID: 21493665; PMCID: PMC3077739.[6]Yin TT, Bi Y, Li P, Shen SM, Xiong XL, Gao LJ, Jiang C, Wang Y, Feng WH, Zhu DL. Comparison of Glycemic Variability in Chinese T2DM Patients Treated with Exenatide or Insulin Glargine: A Randomized Controlled Trial. Diabetes Ther. 2018 Jun;9(3):1253-1267. doi: 10.1007/s13300-018-0412-6. Epub 2018 May 9. PMID: 29744819; PMCID: PMC5984915.[7]Henry RR, Strange P, Zhou R, Pettus J, Shi L, Zhuplatov SB, Mansfield T, Klein D, Katz A. Effects of Dapagliflozin on 24-Hour Glycemic Control in Patients with Type 2 Diabetes: A Randomized Controlled Trial. Diabetes Technol Ther. 2018 Nov;20(11):715-724. doi: 10.1089/dia.2018.0052. Epub 2018 Sep 14. PMID: 30222367; PMCID: PMC6208164.
[8]Li FF, Shen Y, Sun R, Zhang DF, Jin X, Zhai XF, Chen MY, Su XF, Wu JD, Ye L, Ma JH. Effects of Vildagliptin Add-on Insulin Therapy on Nocturnal Glycemic Variations in Uncontrolled Type 2 Diabetes. Diabetes Ther. 2017 Oct;8(5):1111-1122. doi: 10.1007/s13300-017-0303-2. Epub 2017 Sep 18. PMID: 28921310; PMCID: PMC5630558.[9]Li FF, Jiang L, Fu L, Zhu HH, Zhou P, Zhang D, Su XF, Wu JD, Ye L, Ma JH. Exenatide Add-on to Continuous Subcutaneous Insulin Infusion Therapy Reduces Bolus Insulin Doses in Patients with Type 2 Diabetes: A Randomized, Controlled, Open-Label Trial. Diabetes Ther. 2017 Feb;8(1):177-187. doi: 10.1007/s13300-016-0222-7. Epub 2016 Dec 19. PMID: 27995593; PMCID: PMC5306121.[10]Li FF, Jiang LL, Yan RN, Zhu HH, Zhou PH, Zhang DF, Su XF, Wu JD, Ye L, Ma JH. Effects of saxagliptin add-on therapy to insulin on blood glycemic fluctuations in patients with type 2 diabetes: A randomized, control, open-labeled trial. Medicine (Baltimore). 2016 Oct;95(43):e5229. doi: 10.1097/MD.0000000000005229. PMID: 27787387; PMCID: PMC5089116.
[11]Marfella R, Barbieri M, Ruggiero R, Rizzo MR, Grella R, Mozzillo AL, Docimo L, Paolisso G. Bariatric surgery reduces oxidative stress by blunting 24-h acute glucose fluctuations in type 2 diabetic obese patients. Diabetes Care. 2010 Feb;33(2):287-9. doi: 10.2337/dc09-1343. Epub 2009 Nov 4. PMID: 19889803; PMCID: PMC2809267.[12]Gorn L, Faradji RN, Messinger S, Monroy K, Baidal DA, Froud T, Mastrototaro J, Ricordi C, Alejandro R. Impact of islet transplantation on glycemic control as evidenced by a continuous glucose monitoring system. J Diabetes Sci Technol. 2008 Mar;2(2):221-8. doi: 10.1177/193229680800200208. PMID: 19885346; PMCID: PMC2771498.
[13]Yin Y, Hao H, Cheng Y, Zang L, Liu J, Gao J, Xue J, Xie Z, Zhang Q, Han W, Mu Y. Human umbilical cord-derived mesenchymal stem cells direct macrophage polarization to alleviate pancreatic islets dysfunction in type 2 diabetic mice. Cell Death Dis. 2018 Jul 9;9(7):760. doi: 10.1038/s41419-018-0801-9. PMID: 29988034; PMCID: PMC6037817.本文首发:医学界内分泌频道本文整理:医学界CDS报道组-妮娜