二甲双胍与中国乳腺癌患者生存结局
然后点右上角“…”菜单,选择“设为星标”

既往研究结果表明,2型糖尿病临床治疗药物二甲双胍服用者的癌症死亡率较低。不过,二甲双胍对中国乳腺浸润癌伴2型糖尿病患者生存结局的影响尚不明确。
2021年5月11日,英国《自然》旗下《科学报告》在线发表河北医科大学第四医院(河北省肿瘤医院)回天立、尚超、杨柳、王美祺、李若阳、宋振川等学者的研究报告,探讨了二甲双胍对中国乳腺浸润癌伴2型糖尿病患者生存结局的影响。
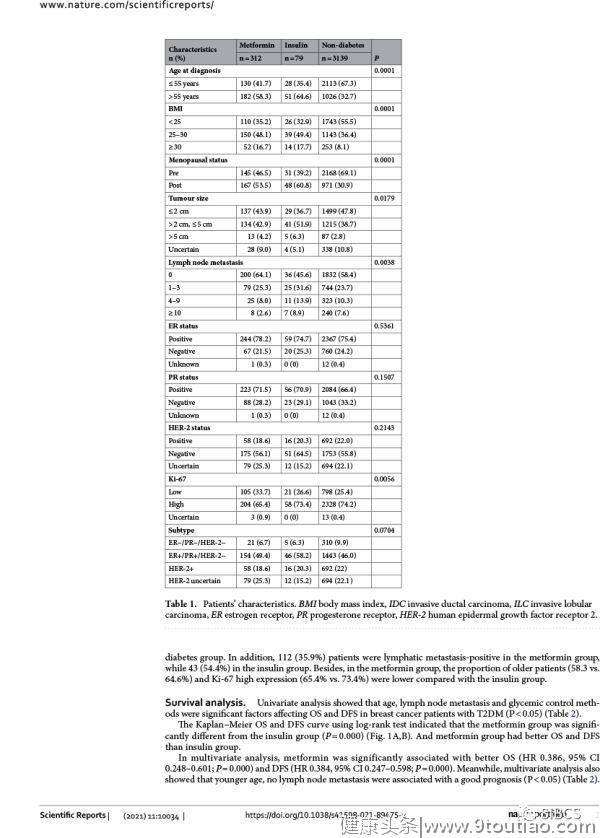
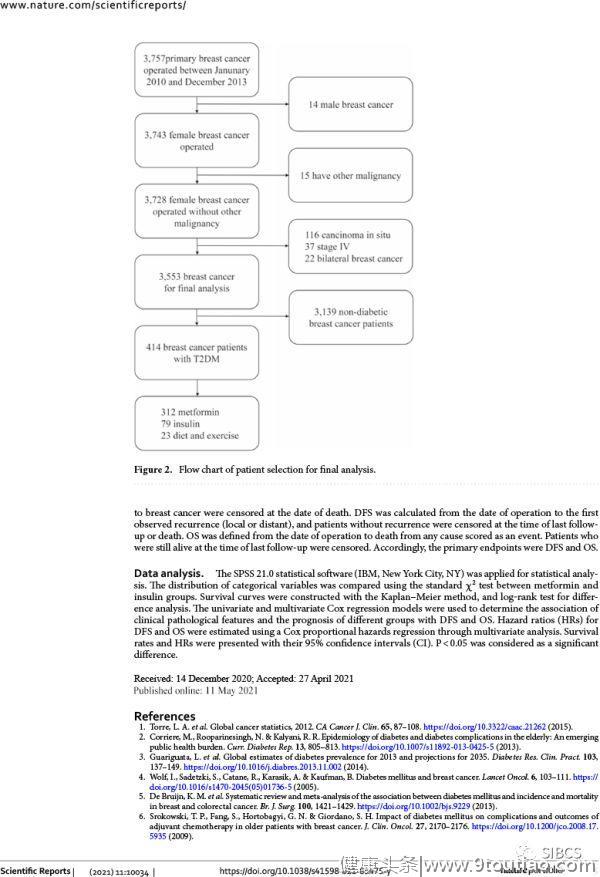
该单中心大样本回顾研究对2010年1月~2013年12月河北医科大学第四医院连续3757例原发乳腺癌手术患者进行回顾分析。剔除男性乳腺癌14例、其他恶性肿瘤15例、乳腺原位癌116例、四期乳腺癌37例,根据药物治疗将其余3553例患者分为非糖尿病组3139例、糖尿病二甲双胍组312例、糖尿病胰岛素组79例、糖尿病饮食锻炼组23例。对无病生存和总体生存随访数据进行生存曲线分析和对数秩检验。对诊断时年龄、体重指数、肿瘤大小、淋巴结转移数量、雌激素受体状态、孕激素受体状态、增殖指数Ki-67、是否糖尿病、糖尿病治疗药物进行多因素比例风险回归模型预后分析。
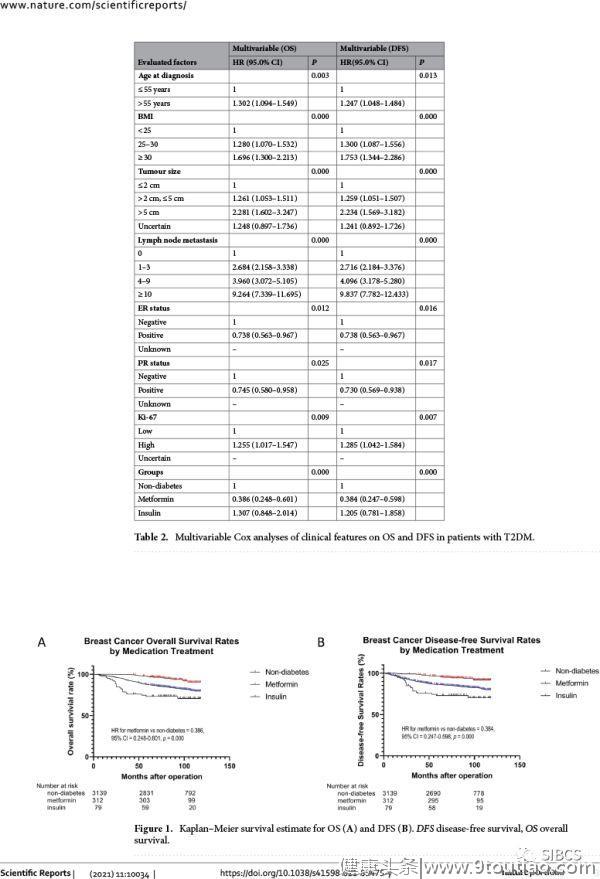
结果,非糖尿病组、二甲双胍组、胰岛素组的生存差异显著:
5年无病生存率:85.8%、96.1%、73.0%(P
5年总体生存率:87.3%,97.1%、73.3%(P
多因素比例风险回归模型预后分析表明,二甲双胍是无病生存和总体生存的独立预后因素,无论其他预后因素如何。
因此,该单中心大样本回顾研究结果表明,二甲双胍对中国乳腺浸润癌伴2型糖尿病患者的生存结局可能具有良好影响,故有必要进一步开展多中心大样本前瞻研究进行验证。
Sci Rep. 2021 May 11;11(1):10034.
Metformin improves the outcomes in Chinese invasive breast cancer patients with type 2 diabetes mellitus.
Hui T, Shang C, Yang L, Wang M, Li R, Song Z.
Hebei Medical University Fourth Affiliated Hospital, Shijiazhuang, China.
Early reports indicate that metformin, a clinical drug administered to treat type 2 diabetes mellitus (T2DM), was found to be associated with a better prognosis of cancer. The objective of this study was retrospectively analyzed the effect of metformin on the outcomes of Chinese breast cancer patients with T2DM. A total of 3757 primary invasive breast cancer patients who underwent surgery from January 2010 to December 2013 were enrolled. According to the medication treatment, all the patients were divided as non-diabetes group, metformin group and insulin group. The follow-up data for disease-free survival (DFS) and overall survival (OS) were obtained from 3553 patients (median follow up of 85 months) and estimated with the Kaplan-Meier method followed by a log-rank test. Multivariate Cox proportional hazards regression model was applied. The results showed that there was a significant survival difference among non-diabetes group, metformin group and insulin group, 5-year DFS was 85.8%, 96.1%, 73.0%, and 5-year OS was 87.3%, 97.1%, 73.3% respectively (P